The Neonatal-Perinatal Medicine Fellowship at Dell Medical School has taken input from the neonatal faculty and associated specialties to design a curriculum with all the best components of training that the program’s leaders have experienced nationally and internationally.
Curriculum Components
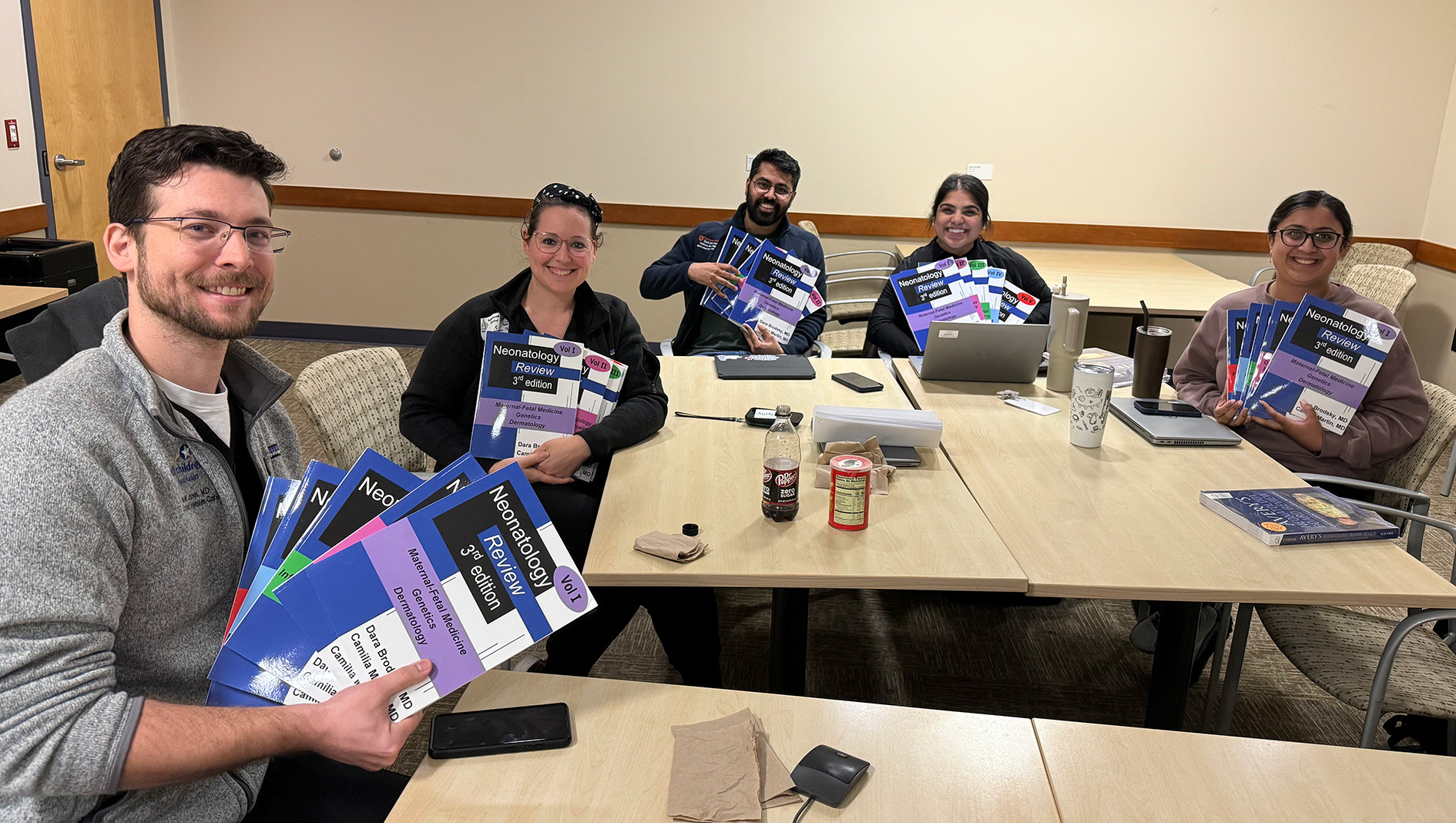
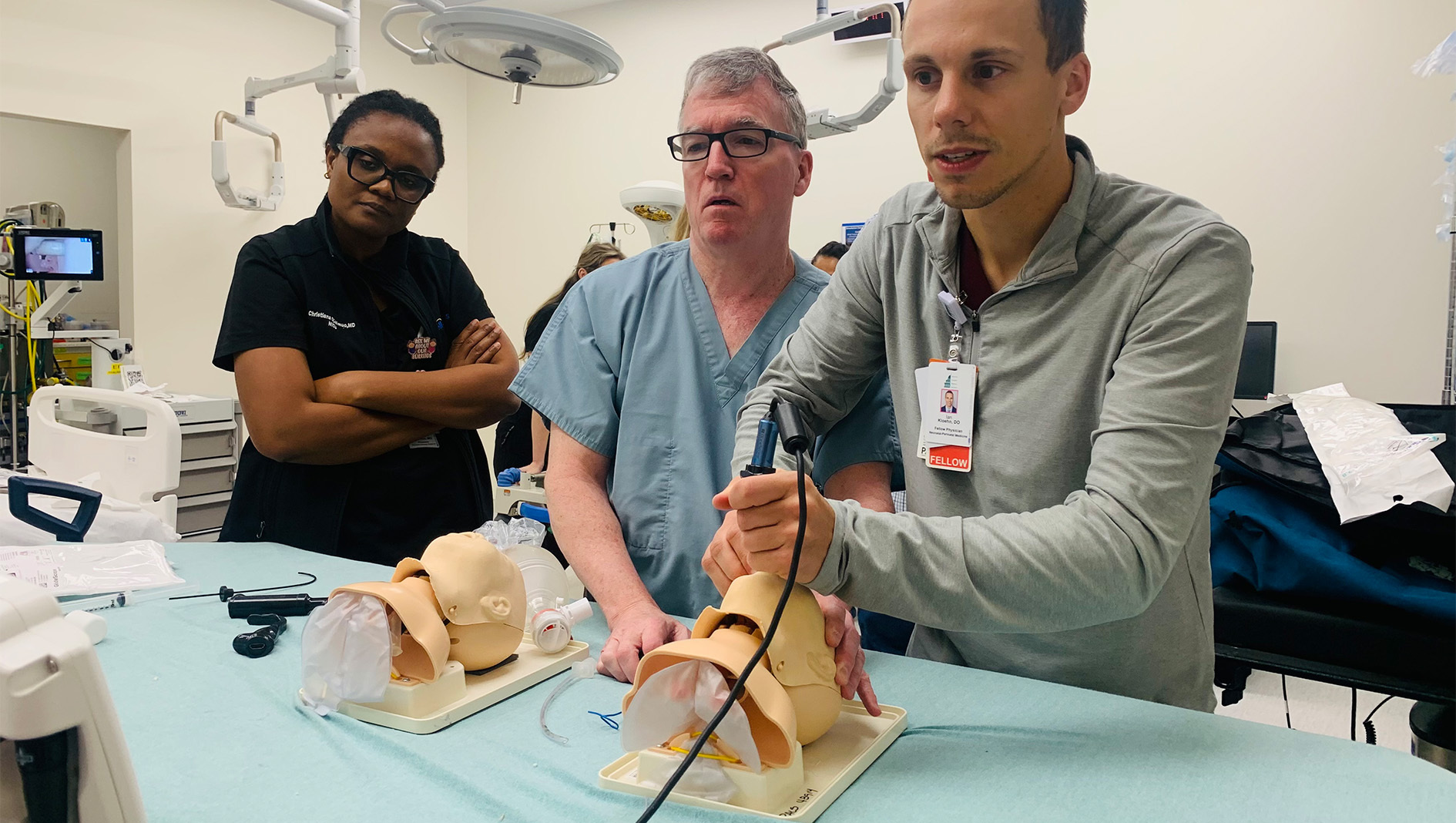
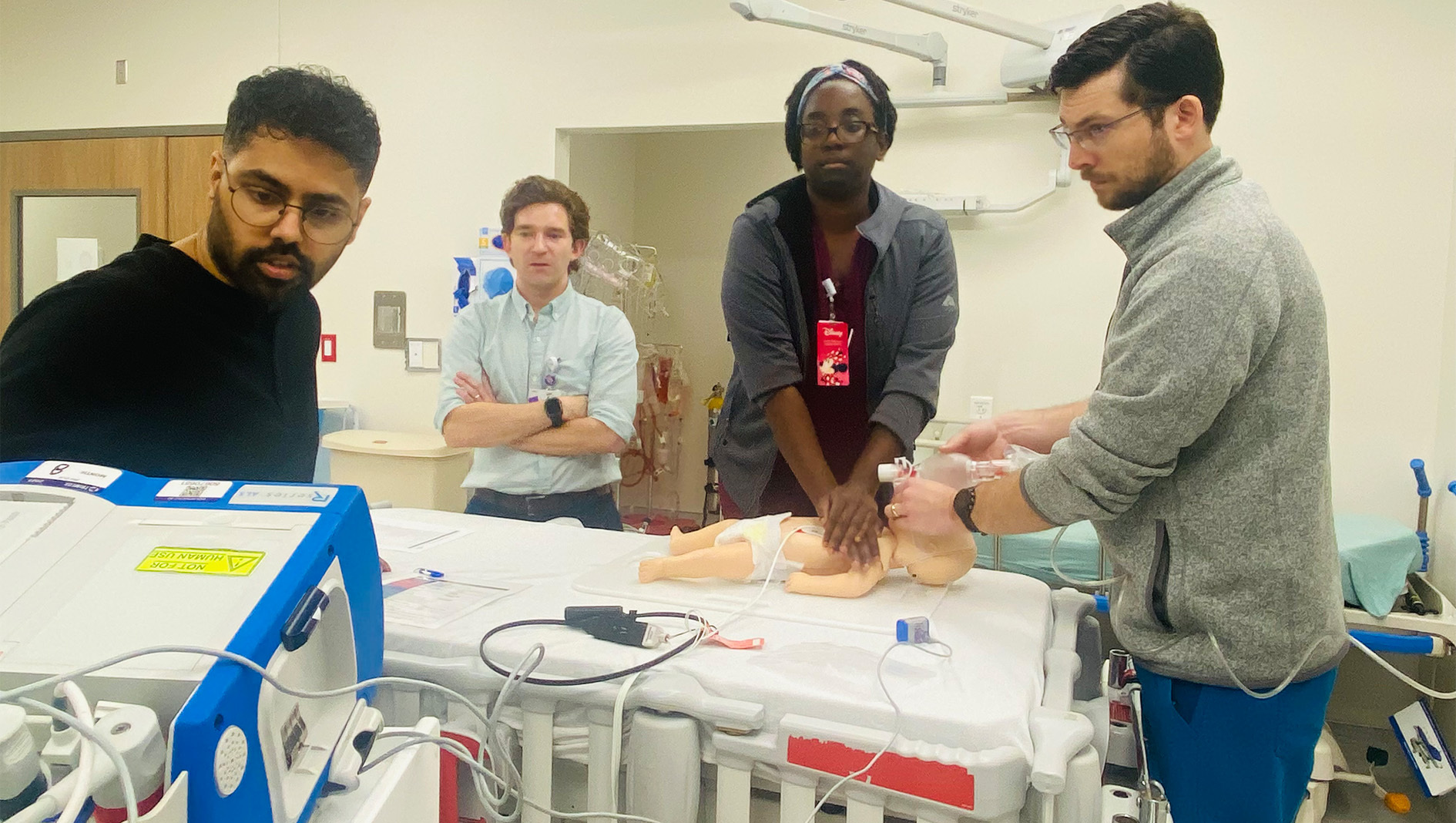
Clinical training in the Neonatal-Perinatal Medicine Fellowship is grounded in applied physiology. First-year fellows spend the month of July in a comprehensive four-week bootcamp that includes simulation, didactics learning and procedural training. Fellows receive a comprehensive primer on the physiology and pathophysiology of the fetus and newborn utilizing a flipped classroom interactive format coupled with hands-on skills training. Weekly Wednesday afternoon sessions serve as the foundational curriculum for fellows. This time is prioritized and protected by neonatal faculty taking over all clinical responsibility during teaching.
Weekly teaching is supplemented with a wide range of educational conferences including neonatal case conference, fetal care conference, quality assurance (formerly morbidity and mortality), journal club, neonatal grand rounds, pediatric grand rounds, cardiac center conferences and fellows college (attended by all Dell Children’s pediatric fellows.)
Clinical Rotations
On-service clinical rotations take place at both Ascension Seton Medical Center Austin and Dell Children’s Medical Center, and are taken in a combination of two- and four-week blocks to give an opportunity to follow the natural history of neonatal conditions.
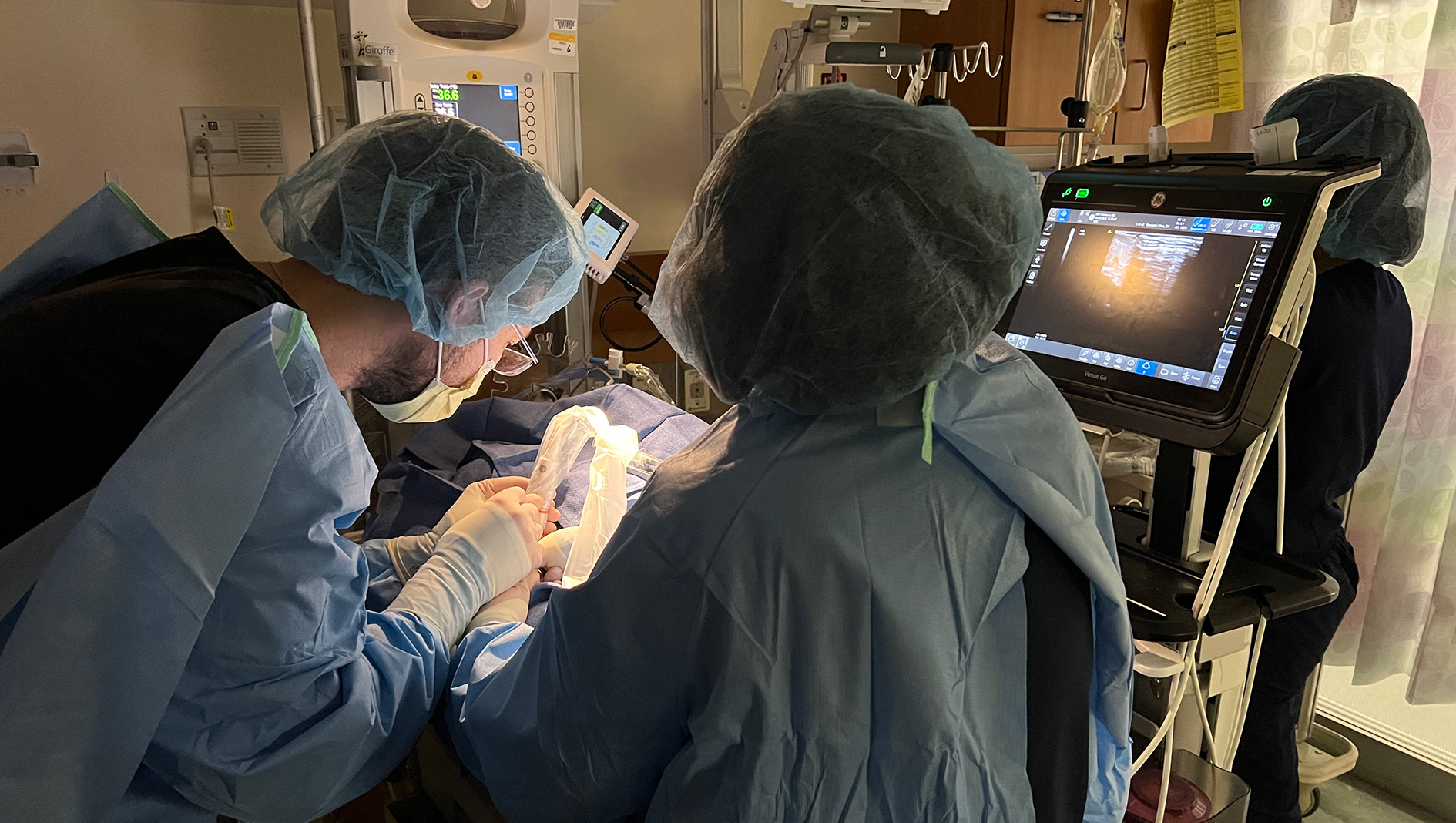
In each service block clinical rotation, fellows are paired with a neonatology attending physician for two weeks to provide consistency of supervision. Specific learning goals are discussed at the beginning, middle and end of each rotation, with written feedback also provided at the end of each rotation. Feedback will not only focus on clinical knowledge but also the essential skills needed for a successful independent neonatal practice. These include communication with families and care-team providers, systems-based care with cost-conscious decision-making, procedural skills, teaching skills and leadership (as appropriate based on year of training).
Clinical rotations are concentrated in the first two years of the program to allow maximal time for research and scholarly activity later in training. Fellows in their second year also complete blocks in cardiac intensive care and in maternal fetal medicine. In the third year, fellows will have two four-week “co-attending” blocks where they are expected to run the clinical service with a faculty member immediately available for support.
Fellow Schedules & Overnight Call
Fellows have the autonomy to create their own block and overnight call schedules with review and approval by the program director. Fellows are required to take 50 calls per year and self schedule these equally between Ascension Seton Medical Center (level 3 NICU) and Dell Children’s (level 4). Overnight calls may be taken during both service and research blocks and are scheduled on all nights except Tuesday to allow fellows protected time to attend Wednesday didactics.
Annual vacation (three weeks per year) can be taken during any of the research call blocks. Protected time for board preparation is available for the four weeks leading up to the pediatric board exams. For fellows who have already completed pediatric boards, this time can be used for additional research or electives. Four four-week blocks of elective time are allotted. These can be used by fellows in any combination and can be used for research, additional clinical time or a range of educational experiences.
Program Strengths
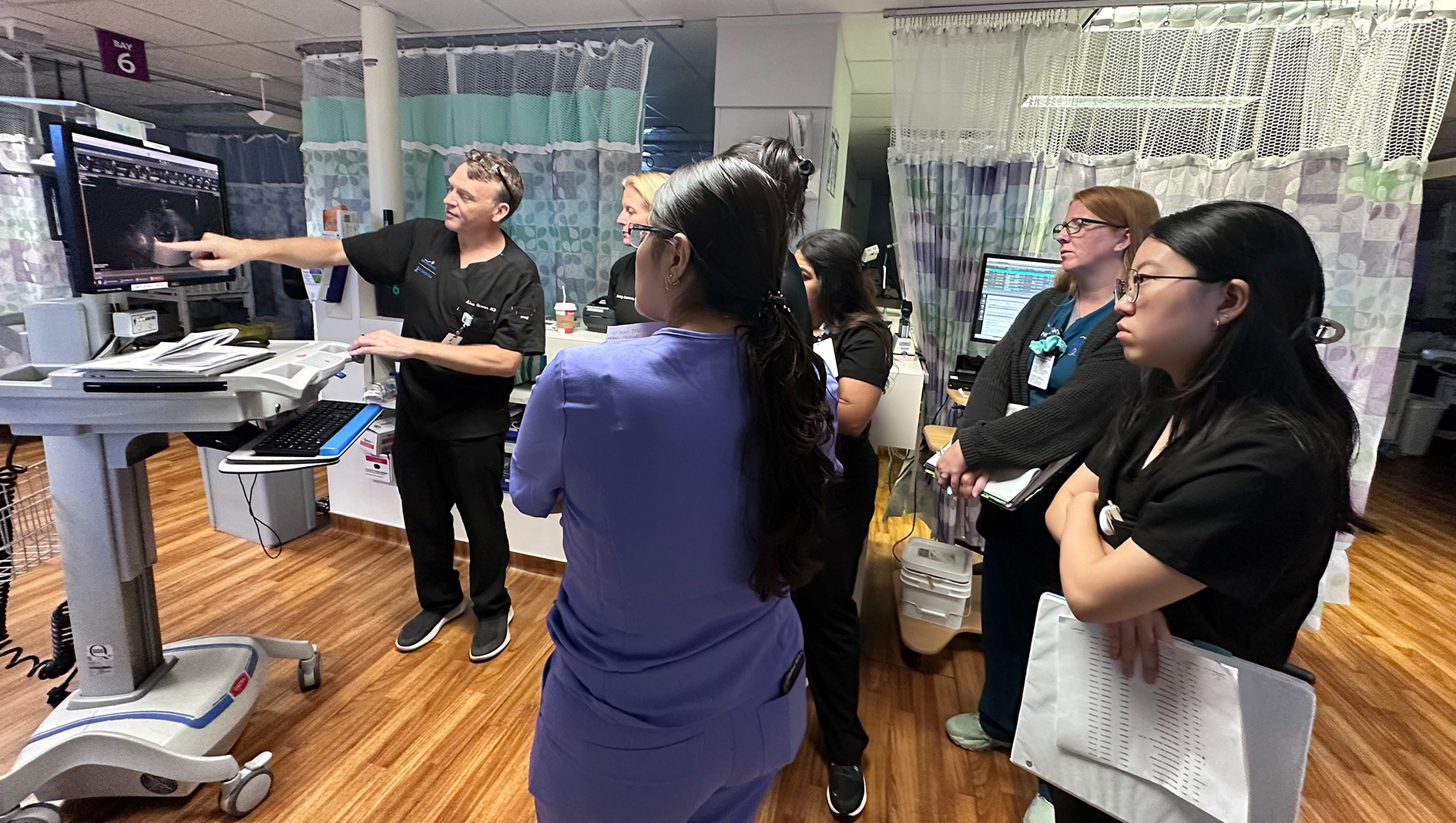
Point-of-care ultrasound: Point-of-care ultrasound (POCUS) has dramatically expanded its footprint in the NICU in the last decade. All fellows will be expected to acquire basic POCUS skills (vascular access, pleural/pericardial effusion, cardiac filling/function) with elective and research time allowing more in-depth skills acquisition in diagnostic and procedural POCUS and targeted neonatal echocardiography (TNE). The ultrasound program is led by Alan Groves, M.D., who has substantial experience in both POCUS and TNE. Groves maintains a leading website in POCUS education, has initiated POCUS programs in multiple NICUs and is the course director for the Annual Neonatal and Pediatric POCUS course hosted jointly with Children’s Hospital of Philadelphia in Austin.
Global health: Collaborating with the UT Global Health Program, this training promotes education, research and service to promote health equity for vulnerable populations. UT Austin currently has training partnerships with Kenya and Mexico. Members of our neonatal division also have partnerships with Guatemala and Egypt. With appropriate advance notice and administrative approvals, other sites can be considered for clinical rotation and research.
Vital sign analytics/biomedical engineering/technology development: This training collaborates across multiple departments with a focus on advancing understanding of the pathophysiology of diseases and developing and applying biosensors to track and predict health. Our NICU team has a close collaboration with David Paydarfar, M.D., chair of the Department of Neurology, whose research focuses on predictive analytics and assessment of motion as a vital sign. A number of partnerships with the Cockrell School of Engineering provide opportunities for development and commercialization of novel devices with support from UT Austin’s Discovery to Impact Team.
Advocacy: Mentorship in advocacy is available through the Dell Medical School Department of Pediatrics Advocacy Committee, which focuses on legislative policy, education, community outreach, social determinants of health, innovation solutions and research. A multi-specialty team of pediatric faculty, trainees and staff participate in IRB-reviewed advocacy initiatives at the institutional and community level. The proximity to the Texas State Capitol also affords many opportunities for trainees in legislative and health policy advocacy. Members of the neonatology faculty active in state and national organizations serve as mentors for trainees interested in future health policy careers.
Health economics and administration: This elective offers practical exposure to the leadership, management and strategic-development skills required to guide an expanding multisite neonatology service. Through existing state-wide clinical and quality-improvement mechanisms, fellows will gain insight into regionalization of care and collaborative efforts among health care systems. Fellows interested in becoming a medical director, division chief or hospital administrator are encouraged to take this elective and work closely with John Loyd, M.D., MPH, Molly Pont, M.D., and Mitchell Imm, M.D.
Ethics: All fellows receive a primer in basic ethical concepts and principles beginning in month one of the program. Additional focus through participation in an ethics elective allows for an in-depth review of important historical cases and their respective precedents, bedside instruction in the practical application of clinical bioethics and attendance at ethics meetings and leading case discussions. Fellows participating in this elective work closely with faculty facilitators, Chris Klunk, M.D. and Pat Hodges, M.D.
Palliative care: This training provides experience in the active and total care of infants with life-limiting conditions, with a focus on enhancing quality of life, managing symptoms and supporting families across multiple specialties and embracing physical, emotional, social and spiritual elements.
Mentorship
Onboarding mentorship: Our Neonatal-Perinatal Medicine Fellowship Program is highly committed to providing adequate mentorship for our fellows. Our incoming fellows will initially receive onboarding mentorship and guidance for the first two months. This mentorship is provided by the program leadership. The goal is to ensure a smooth transition from residency to fellowship and acclimation to the health system.
Clinical and academic mentorship: Fellows are expected to select a clinical mentor within the first six months of training. This formal and structured mentorship ensures successful progression throughout the fellowship training. The faculty mentors assist our fellows with developing an individualized learning plan to support the fellows’ career development. Mentors provide feedback to ensure competencies in the core areas including patient care, medical knowledge, professionalism, scholarship, and system and practice-based learning are achieved. The fellows meet with their mentors at least twice a year to review evaluations and trainee goals. The program requires faculty mentors to be available for check-ins and frequent meetings as necessary to support the fellow.
Research mentorship: Every fellow will have a primary research mentor plus mentorship from their scholarly oversight committee (SOC). Each fellow will work with their primary research mentor and program leadership to form their SOC, composed of three members and one must be from outside the Division of Neonatology. Fellows are required to meet with their SOC a minimum of once in the first year and twice in each year thereafter to discuss progress on scholarly projects. With SOC and program leadership approval, fellows can design unique research experiences aligning with their career path and goals.
Dell Medical School Advanced Training Opportunities for Fellowship
Advancing Care Transformation: Dell Med’s graduate medical education office offers the Distinction in Care Transformation program through its Advancing Care Transformation signature curriculum to residents and fellows at no cost. The program is focused on equipping students to tackle systemic challenges in health and lead change in an evolving health care landscape.
Fellowship in medical education: This two-year program aims to develop medical educators who lead, create, teach, and evaluate educational initiatives.
UT Austin Masters Programs
Funding for masters programs is currently not available through Dell Medical School or the Pediatric Department though some tuition assistance may be available and programs may work with candidates to help obtain funding. In general, fellowship programs will consider providing protected time for studying for a higher degree, and can consider having degree work count towards ABP scholarly requirements and internal research requirements.
Masters in Public Health: A number of MPH programs are available with online learning from UT Health Houston.
Master of Science in Health Care Transformation: This one-year program equips health professionals with the skills needed to design and lead health care services that achieve better outcomes.
Master of Arts in Design Focused on Health: A 10-month program which aims to help learners apply strategic design thinking to understand the needs of people seeking health services, receiving care and delivering care.