Asthma-related emergency department visit rates for local Black and Latinx children are typically higher than for white children, but Dell Med researchers found that disparity lessened significantly during the pandemic — a shift that may be connected to the common cold.

AUSTIN, Texas — Vulnerability to upper respiratory viruses such as flu and the common cold may help explain significant racial and ethnic disparities among children suffering from asthma, according to a new study published in The Journal of Allergy and Clinical Immunology.
Lead author Darlene Bhavnani, Ph.D., is an assistant professor of population health at Dell Medical School at The University of Texas at Austin. She and her team compared emergency department visit rates associated with asthma in Black, Latinx and white children living in Travis County before, during and after COVID-19 prevention efforts went into effect.
“Looking at the data, we made two main observations,” said Bhavnani, who is also an infectious disease epidemiologist in the Biomedical Data Science Hub at Dell Med. “One is that the circulation of upper respiratory viruses in our community went down during the height of stay-at-home orders. The second is that disparities in asthma exacerbations between children of color and white children were dramatically reduced at the same time.”
Key findings of the study include:
- Black children had nearly a sevenfold higher rate of ED visits than white children did during the spring of 2019. This ratio decreased to twice as high during the spring of 2020 after pandemic mitigation efforts went into effect, then increased again to five times as high during spring 2021, when those measures were lifted and respiratory virus circulation increased.
- Latinx children had a twofold higher rate of ED visits than white children did during the spring of 2019. The two groups had similar rates in 2020, but the rate among Latinx children was nearly 1.5 times as high as that of white children during spring 2021.
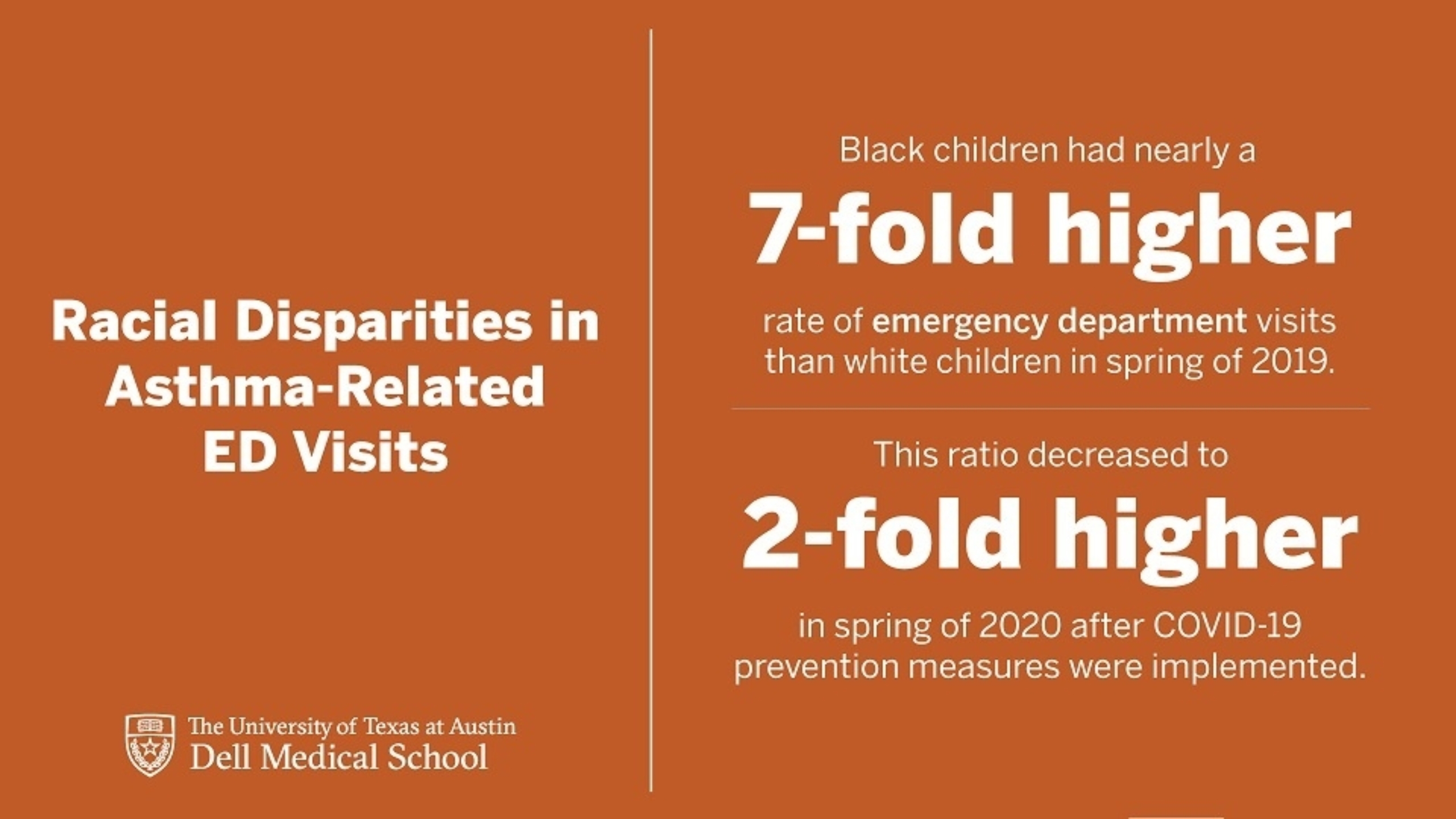
Black children had nearly a sevenfold higher rate of ED visits than white children did during the spring of 2019. This ratio decreased to twice as high during the spring of 2020 after COVID-19 prevention measures were implemented.
“The reduction in racial and ethnic differences in ED visit rates when circulation of upper respiratory viruses was reduced raises the question of whether these viruses are driving some of the disparities we see in asthma exacerbations outside of pandemic periods,” said Bhavnani.
Based on these results, senior author and pediatrician Elizabeth Matsui, M.D., says the focus now is on investigating why Black and Latinx children may be more vulnerable to upper respiratory viral infections such as flu, rhinovirus, RSV and adenovirus.
“We need more research to test this hypothesis and to identify contextual factors that may underlie an increased vulnerability to these seasonal viruses,” said Matsui, who is the associate chair for research in the Department of Population Health and a professor in the departments of Pediatrics and Population Health at Dell Med. “It could be that they’re more exposed. It could be that they’re more susceptible or that they have more severe infections that lead to exacerbations.”
Next, Bhavnani and her team will examine the social and environmental factors that may play roles in the increased vulnerability to upper respiratory viruses.
For example, there may be challenges at the neighborhood level that lead to a child being exposed to more viruses at school, such as crowded classrooms and insufficient ventilation.
“There’s also research that links air pollution and exposure to certain allergens to increased susceptibility to viral infection that we’re just now starting to appreciate,” said Bhavnani. “If we can learn more about the connections between the environment and our health, we can start to think about how to reduce these pervasive disparities.”