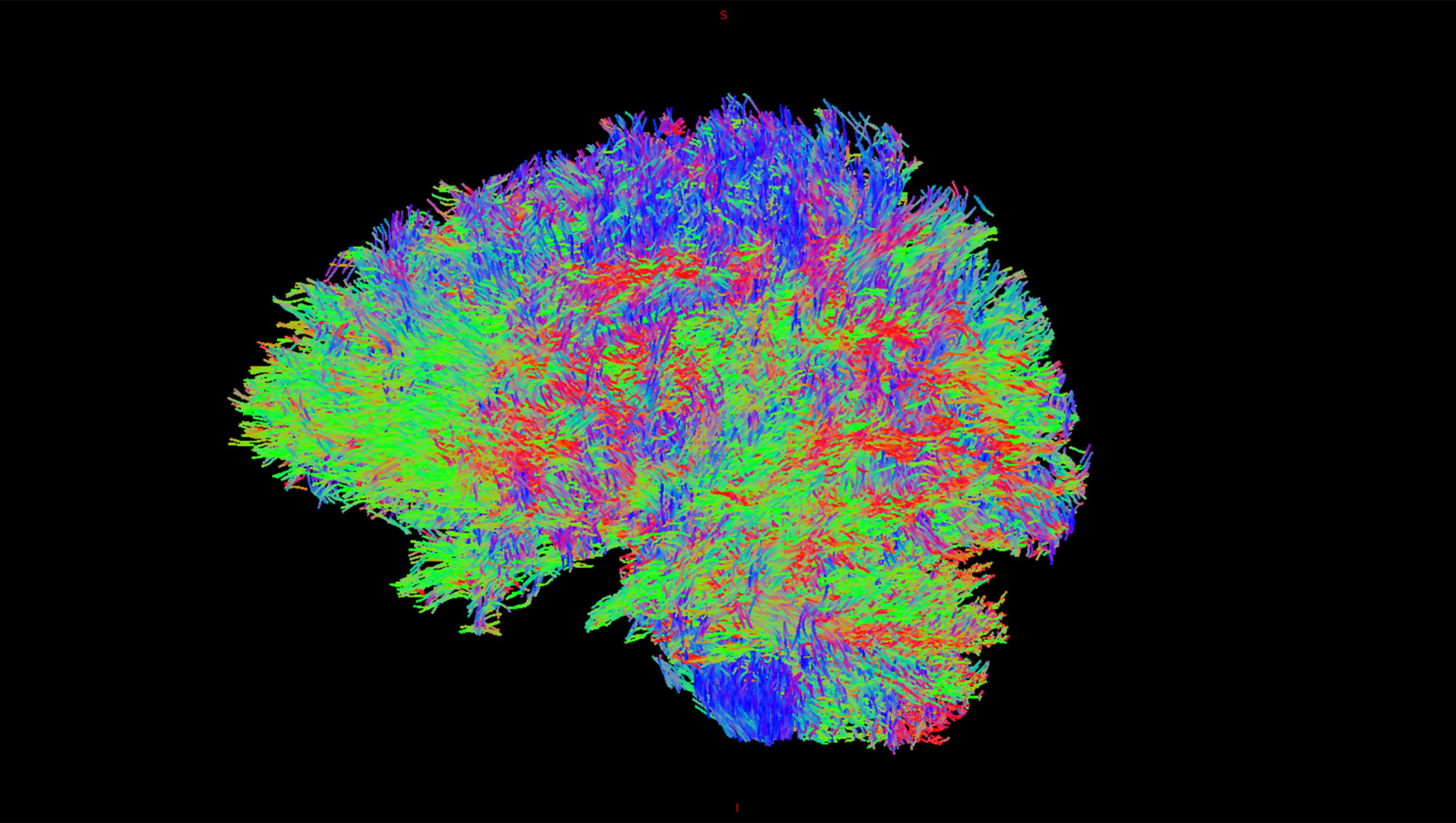
A diffusion weighted image shows the movement of water molecules within brain tissue. Courtesy: Mulva Clinic for the Neurosciences.
Researchers at Dell Medical School at The University of Texas at Austin are using state-of-the-art neuroimaging techniques and artificial intelligence to identify changes in the brains among children of adults living with bipolar disorder — a debilitating condition that interferes with daily life due to its dramatic mood, energy and activity level shifts.
Almost 3% of U.S. adults live with bipolar disorder, one of the leading causes of disability worldwide. The highest risk factor for bipolar disorder is having a close family member with the condition. Understanding the pathophysiology of the disease and how it changes over time means researchers may lead to more effective treatment in earlier phases of the illness, which could then improve long-term outcomes.
“We are trying to understand how the brain’s different regions connect to each other, and what’s fueling the brain’s reward system,” said investigator Jorge Almeida, M.D., director of the Bipolar Disorder Center at Mulva Clinic for the Neurosciences and associate professor in the Department of Psychiatry and Behavioral Sciences at Dell Med. Charles Nemeroff, M.D., Ph.D., director of Dell Med’s Institute for Early Life Adversity Research, is a co-investigator in the study, contributing specifically on understanding the impact of childhood trauma on brain development. Stephen Strakowski, M.D., Professor of Psychiatry at Indiana University and Dell Med, and Melissa DelBello, M.D., Chair of Psychiatry at the University of Cincinnati, co-lead the study.
“The brain has too much energy being delivered by its reward system in bipolar disorder, which affects the brain’s ability to regulate the amount of energy driving it to act. That’s what causes the symptoms of mania in bipolar disorder,” says Almeida. “It’s an imbalance similar to having too much gas and not enough brakes,” he explains.
The brain’s inability to “hit the brakes” results in manic behaviors such as spending too much money, engaging in risky behaviors and sleep loss or disruption, says Almeida.
In Search of a Better Understanding of the Brain’s Connections
According to Almeida, the study is the first of its kind to focus specifically on the progression of the disease over time via neuroimaging in children of parents with bipolar disorder.
The research leverages AI algorithms to discern variations in participants’ brains, combining imaging data with cognitive, clinical, early life adversity and psychosocial function measures. The result is a precise delineation of brain maturation for each person at risk of developing bipolar disorder, says Almeida.
The five-year longitudinal study uses functional magnetic resonance imaging (fMRI) to identify early signs that the brain is developing bipolar disorder. Participants ages 14 to 21 — a critical time when mania symptoms often develop — undergo annual brain scans to track changes in the brain. If they become depressed, suicidal or experience mania, the participants undergo additional brain scans to help researchers understand how the damage is unfolding.
Participants also undergo mood assessments and are required to perform tasks that activate and test the brain’s reward system.
“This study evokes hope for me,” says Almeida. “Hope that we finally have the tools to help this condition and possibly prevent it from ever happening.” In its third year of a five-year grant, the research is in collaboration with the University of Cincinnati and is funded by the National Institute of Mental Health.