From muscle weakness to poor sleep and vision problems – aging takes a toll on the body, especially for older people who have multiple sclerosis. New research by UT Health Austin’s Léorah Freeman, M.D., will help meet the needs of older patients and shed light on how MS changes with age.
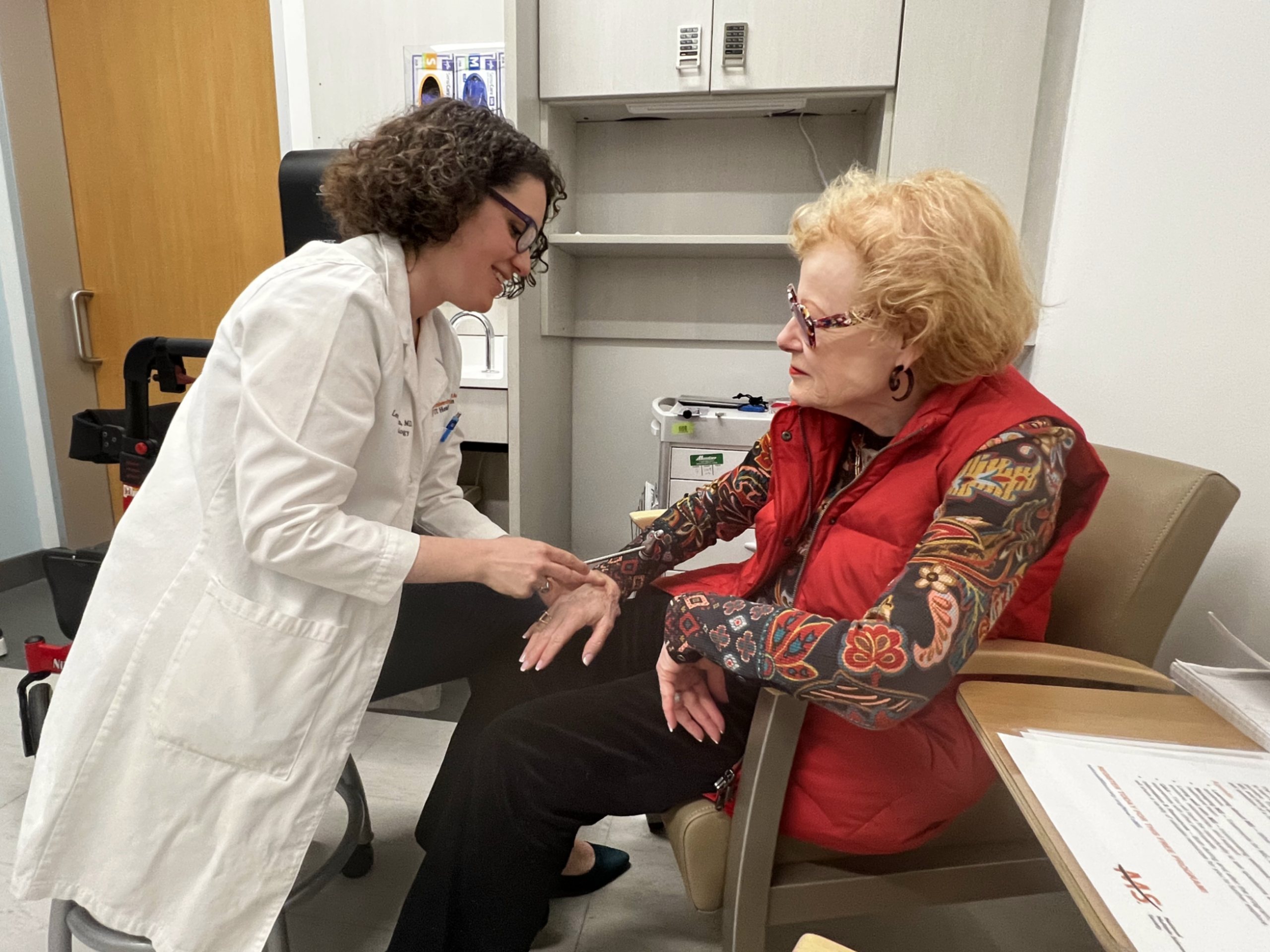
Léorah Freeman, M.D., Ph.D. (left), treats one of her patients, 70-year-old Vicki Aymond. Aymond was diagnosed with multiple sclerosis in 2010.
AUSTIN, Texas — The symptoms of multiple sclerosis, or MS, can sometimes mirror the normal signs of aging, such as muscle weakness, balance problems, fatigue, vision changes and sleep disturbances. Because MS can lead to lasting disability and pain, resulting in the loss of the ability to write, speak or walk, it’s important to better understand the needs of patients and challenges of the disease within the context of aging.
However, relatively little research focuses on people older than 50 with MS. At Dell Medical School at The University of Texas at Austin, Léorah Freeman, M.D., Ph.D., and her team are working to change that. Freeman is an assistant professor and director of the Multiple Sclerosis Imaging and Outcomes Research Laboratory. She also cares for patients in the Multiple Sclerosis and Neuroimmunology Center at UT Health Austin, Dell Med’s clinical practice, and leads the school’s Healthy Aging with MS research initiative and clinical program.
MS changes with age, increasing the complexity of care for older patients, who are not only at higher risk of progression of the disease, when symptoms accumulate and worsen without alleviating, but are also more susceptible to complications from therapies that suppress the immune system. While caring for older people with MS, Freeman gathers data to identify predictive biomarkers of disease progression and response to therapies in this age group. The goal is to establish best practices for the management of MS in older adults, and to build a novel multidisciplinary clinic fully integrated with a research program.
Vicki Aymond, 70, experienced the challenges of being diagnosed with MS as an older adult. Initially, Aymond struggled to receive a correct diagnosis. Physicians told her she was just getting older when she described her symptoms. “But it wasn’t that at all,” said Aymond. “I know myself. I know my body. I should not be walking out of this room and bumping into the wall. Everything could not be attributed to the fact that I was just getting older.”
Seeing Freeman, a physician with specific experience in older adults with MS, has made a difference for Aymond, who was also diagnosed with breast cancer at the start of the pandemic. This complicated her care. “As you get older, you’re more likely to have comorbid conditions,” said Freeman. “You can have cancer. You can have dementia of other causes. You can have neuropathies or cardiovascular disease. Taking a broad view is important when we look at the aging population because MS can explain a lot, but it doesn’t always explain everything.”
If we can bring a team to meet the needs of older adults with MS, then we’re not only listening one-on-one, but we’re listening collectively. We can make a huge difference in the coordination of care.
—Léorah Freeman, M.D., Ph.D.
Freeman’s goal is to “focus on the right approach for each of the symptoms that people present so that they can thrive,” she said. “The vision for our Healthy Aging with MS program is to deliver care that is specifically tailored to the needs of people living with MS as they get older,” Freeman said. “At the same time, our goal is to answer the research questions that matter most to our patients and to provide meaningful education to help them on their journey with MS.”
On the clinical side, Freeman and her team hope to build a more comprehensive and collaborative model of care — specifically tailored to the needs of older people. To better understand these needs, Freeman will hold focus groups with patients to discuss how they would like their care structured and delivered. Freeman also plans to launch research projects that investigate what drives MS progression and disability in older adults and explore the risks associated with multiple medications prescribed to older patients with MS.
Inspiring Philanthropic Support
Freeman’s research-driven approach to MS care resonated with McCombs School of Business alumnus and former PepsiCo and Yum! executive Greg Moore. Together with his late wife, Kathy Moore, he established the Kathleen C. Moore Foundation, which is dedicated to funding research and resources to fight, cure and eliminate MS. Kathy Moore, a 1971 UT psychology alumna, was diagnosed with MS at age 33 and lived with the disease for almost 20 years until reaching the secondary progressive stage in 2010. She died from MS in 2019, and today her family honors her legacy through the work of the foundation, where Greg Moore serves as president and CEO.
In September, the foundation made a $1 million gift to Dell Med to establish the Kathleen C. Moore Research Fund for Hope in her memory. Under Freeman’s direction, the fund will support MS-focused research and programming.
For Moore, the gift was a way to reconnect with his alma mater and support a cause that profoundly shaped his life. The fund will “shed light on how MS changes with age and help us understand the unmet needs of older adults with MS — a population that has been largely underrepresented in research to date,” he said.
“This kind of support, with a commitment to research and clinical care, is helping us to better understand MS, which in turn supports our ability to provide more comprehensive care,” said David Paydarfar, M.D., chair of Dell Med’s Department of Neurology and director of the school’s Mulva Clinic for the Neurosciences. “The Kathleen C. Moore Research Fund for Hope will transform the lives of patients and families affected by MS, and it is an incredible, enduring tribute to Kathy.”
“Dr. Freeman’s work fits perfectly into the foundation’s mission,” said Moore, whose vision is to help people with MS lead more independent and fulfilled lives, and to support world-class MS care for patients in Austin.
Freeman works alongside fellow MS specialists Ethan Meltzer, M.D. and Duriel Hardy, M.D.; along with a multidisciplinary team that includes a physician assistant, social worker, nurse, clinical pharmacist and dietitian. “If we can bring a team to meet the needs of older adults with MS, then we’re not only listening one-on-one, but we’re listening collectively,” said Freeman. “We can make a huge difference in the coordination of care.”